The demographics of a professional population and its value marketers and providers. A glimpse at the future of the US physician in 2023.
Physicians play a critical role in the $4.3 trillion US healthcare system as gatekeepers for patients, insurers, and pharmaceutical companies. They have extensive educations, earn high incomes, and work longer hours than most other professionals do. They’ve also endured significant stress over the course of the pandemic, and burnout is pervasive. But it’s not just the medical landscape that’s changing. A new crop of younger and more diverse doctors is emerging.
 Key Takeaways
Key Takeaways
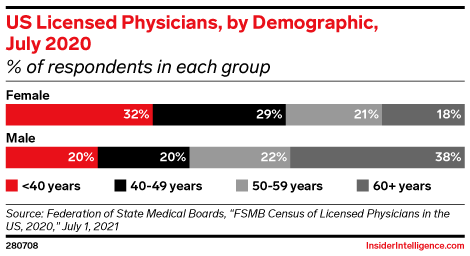
US doctors are becoming more diverse in terms of race and gender. Physicians 50 and older are predominantly white and male, but those younger than 50 are predominantly female.
![]() The “old guard” is changing in the medical profession. For pharma marketers, that means connecting with younger doctors through the media channels they prefer, like social and video. For providers and employers, it means addressing the needs and expectations of a younger, more female population.
The “old guard” is changing in the medical profession. For pharma marketers, that means connecting with younger doctors through the media channels they prefer, like social and video. For providers and employers, it means addressing the needs and expectations of a younger, more female population.
![]() The lack of diversity likely affects patients more than it does marketers or employers, as patients may forgo care if they feel they can’t effectively communicate with their physicians or find ones who understand their background. For employers and providers, leaving racial and ethnic disparities in their staff unaddressed can result in patient loss and declining revenues.
The lack of diversity likely affects patients more than it does marketers or employers, as patients may forgo care if they feel they can’t effectively communicate with their physicians or find ones who understand their background. For employers and providers, leaving racial and ethnic disparities in their staff unaddressed can result in patient loss and declining revenues.
![]() Employers and providers should watch the trends that could impact the recruiting landscape. Doctors who are unhappy with their current employment situation could find that local hospitals aren’t hiring now. Some may be willing to relocate to a provider in a smaller market to find the work-life balance they’re looking for—at a salary they’ll accept.
Employers and providers should watch the trends that could impact the recruiting landscape. Doctors who are unhappy with their current employment situation could find that local hospitals aren’t hiring now. Some may be willing to relocate to a provider in a smaller market to find the work-life balance they’re looking for—at a salary they’ll accept.
![]() Providers that undervalue their doctors risk losing them to other networks that will offer fair and competitive salaries. Marketers should note that, while doctors are among the highest-paid professionals, they often have student loans, mortgages, and other expenses to consider before discretionary purchases like luxury goods.
Providers that undervalue their doctors risk losing them to other networks that will offer fair and competitive salaries. Marketers should note that, while doctors are among the highest-paid professionals, they often have student loans, mortgages, and other expenses to consider before discretionary purchases like luxury goods.
![]() Employers must tackle doctors’ feelings of being overworked and underappreciated at the organizational level. Investing in technology, particularly the electronic health record (EHR) system, is one place to start. But small gestures go a long way, too. Focus on doctors’ well-being with mindfulness training, gym memberships, or dedicated parking spaces—without violating the Stark Law, of course.
Employers must tackle doctors’ feelings of being overworked and underappreciated at the organizational level. Investing in technology, particularly the electronic health record (EHR) system, is one place to start. But small gestures go a long way, too. Focus on doctors’ well-being with mindfulness training, gym memberships, or dedicated parking spaces—without violating the Stark Law, of course.
![]() Employers and providers should be using technology to lighten physicians’ daily workload. Through OpenAI’s ChatGPT, AI is moving into medical offices to handle basic tasks like routing some emails from a doctor’s EHR inbox to the proper administrative level, refilling prescriptions, and answering patient questions about symptoms. Just leave the diagnosing to the doctor.
Employers and providers should be using technology to lighten physicians’ daily workload. Through OpenAI’s ChatGPT, AI is moving into medical offices to handle basic tasks like routing some emails from a doctor’s EHR inbox to the proper administrative level, refilling prescriptions, and answering patient questions about symptoms. Just leave the diagnosing to the doctor.
More doctors are now younger and female.
 More than 1 million professionally active physicians are in the US in 2023.
More than 1 million professionally active physicians are in the US in 2023.
Per January data from the Kaiser Family Foundation (KFF), primary care physicians—internal medicine, family medicine, general practice, pediatrics, OB-GYN, and geriatrics—make up 46.6%. Specialist physicians—psychiatry, surgery, anesthesiology, emergency medicine, and others—make up 53.4%.
 Older males dominate—for now.
Older males dominate—for now.
Today, this population skews male (62.5%), per KFF. The mean age among licensed physicians was 51.7 in 2020, according to the Federation of State Medical Boards (FSMB). The median age of the US population was 38.8 in 2021, per the US Census Bureau.
 More women are attending medical school.
More women are attending medical school.
The share of women entering the medical field has climbed steadily since 2007, from 28.3% of graduates to 37.1% in 2021, per the Association of American Medical Colleges (AAMC). In December 2022, the AAMC reported that women made up the majority (54%) of total US medical school enrollment.
 Men and women choose different specialties.
Men and women choose different specialties.
Men dominate surgical specialties like orthopedic (94.1%), interventional cardiology (91.8%), and thoracic (91.7%), per 2021 data from AAMC. Women gravitate toward family medicine specialties such as pediatrics (65.0%), OB-GYN (60.5%), and geriatric medicine (55.1%).
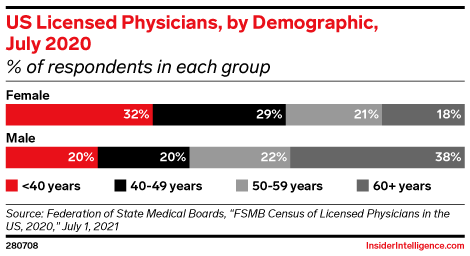
The physician population doesn’t reflect the diversity of the US population.
 Nearly two-thirds (63.9%) of US doctors are white (non-Hispanic).
Nearly two-thirds (63.9%) of US doctors are white (non-Hispanic).
While 57.8% of the US population in the 2020 census was white.
 Just 5.7% of the US population is Asian, but Asians make up 20.6% of doctors.
Just 5.7% of the US population is Asian, but Asians make up 20.6% of doctors.
By contrast, Black people comprise 5.7% of the physician population but 12.1% of the US population; Hispanics, 6.9% of physicians but 18.7% of the population.
 Some positive change is happening in medical school enrollment.
Some positive change is happening in medical school enrollment.
The number of Black students grew 9% in the 2022–2023 academic year, making up 10% of enrollees, per the AAMC. Hispanic enrollment increased 4%, representing 12% of total matriculants.
 The American Medical Association is attempting to address the diversity issue.
The American Medical Association is attempting to address the diversity issue.
The organization is pushing for 14,000 new residency spots for students of color. This could also alleviate the projected shortage of between 37,800 and 124,000 physicians that may occur by 2034.
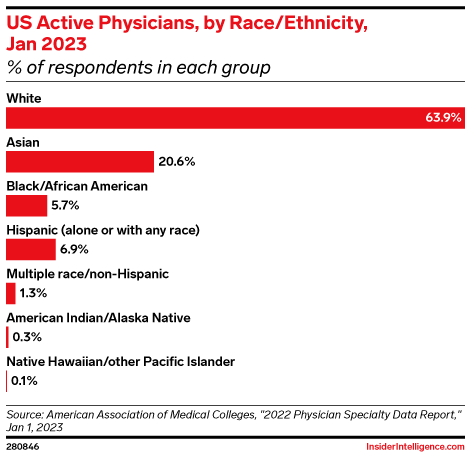
Doctors’ employment landscape is changing.
 US physicians are increasingly leaving their independent practices for networks.
US physicians are increasingly leaving their independent practices for networks.
About 74% are now employees of a health system, a private equity (PE) firm, or a health insurer, per the Physicians Advocacy Institute and Avalere Health. Regulatory and financial pressures, the desire for better work-life balance, and pandemic lockdowns pushed many doctors to sell their practices.
 Many hospitals aren’t financially positioned to hire.
Many hospitals aren’t financially positioned to hire.
Hospitals suffered major operating losses in 2022 amid economic headwinds, and they will still struggle this year, per the February 2023 issue of Kaufman Hall’s “National Hospital Flash Report.” Additionally, recruiting new physicians is becoming less of a priority, as insurers continue to steer patients toward lower-cost care settings.
 PE buyers are targeting the fragmented physician sector.
PE buyers are targeting the fragmented physician sector.
Since 2017, these firms have dominated deals in the medical group sector, per 2023 LevinPro data cited by VMG Health. While they supply administrative and operational support, their primary goal is to build platforms of practices—dentists, primary care physicians, or other specialties—and then sell them to another PE firm, an insurer, or a retailer like CVS Health or Walgreens.
 Employers should beware: Noncompetes may soon disappear—along with their staff.
Employers should beware: Noncompetes may soon disappear—along with their staff.
In January, the Federal Trade Commission (FTC) proposed a rule to ban noncompete clauses in employment contracts. Around 62% of doctors have such a clause, and 87% said they would support the ban, per a March 2023 report by Doximity and Curative. If the rule takes effect later this year, hospitals and other employers could see a mass walkout as doctors defect to competitors.
 Employers should beware: Noncompetes may soon disappear—along with their staff.
Employers should beware: Noncompetes may soon disappear—along with their staff.
In January, the Federal Trade Commission (FTC) proposed a rule to ban noncompete clauses in employment contracts. Around 62% of doctors have such a clause, and 87% said they would support the ban, per a March 2023 report by Doximity and Curative. If the rule takes effect later this year, hospitals and other employers could see a mass walkout as doctors defect to competitors.
Physician salaries are rising, but many still feel underpaid.
The highest-paying jobs in the US are in medicine, per the Bureau of Labor Statistics. Median annual income for physicians in 2022 was $208,000 or higher, depending on specialty. Meanwhile, the median US salary was $54,132. But increased pay for doctors is often disproportionate with their rising stress levels.
 Physician compensation rose in 2022, after stagnating in 2020, due to growing demand for physician services.
Physician compensation rose in 2022, after stagnating in 2020, due to growing demand for physician services.
Primary care physicians earned an average of $260,000 last year, and specialists, $368,000, per an April 2022 report by Medscape. Those figures had increased by 7.4% and 7.0% respectively over 2021.
 High salaries are warranted, especially considering the time and money put toward education.
High salaries are warranted, especially considering the time and money put toward education.
Doctors typically spend four years in an undergraduate program, four more in medical school, then three to seven years in a residency program to learn a specialty before their real earning power kicks in. The average medical school graduate carries $250,990 in total student loan debt.
 But burnout is causing doctors to unionize.
But burnout is causing doctors to unionize.
This has been caused by poor working conditions, excessive workloads, and unsatisfactory compensation. In 2023 alone, staff at Loma Linda University Health, Penn Medicine, George Washington University School of Medicine and Health Sciences, and Mass General Brigham signed up to form unions.
Physician burnout isn’t going away, even if the pandemic eventually does.
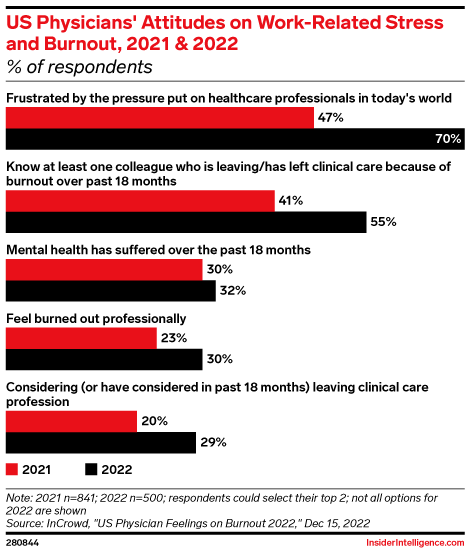
The pandemic, among other factors, added to feelings of depression and exhaustion among physicians. But burnout was an issue long before the pandemic started.
 Doctors feel overworked, even though their workweeks are shorter than they were 20 years ago.
Doctors feel overworked, even though their workweeks are shorter than they were 20 years ago.
Average weekly work hours declined between 2001 and 2021, from 52.6 to 48.6 hours per week, according to a JAMA Internal Medicine study published in December 2022.
 Doctors saw more patients than ever in 2022.
Doctors saw more patients than ever in 2022.
Particularly in primary care settings, per the January 2023 issue of Kaufman Hall’s “Physician Flash Report.” Although that meant more revenues for providers and self-employed doctors, increased expenses and inflation ate into profit margins. Physicians who feel burned out won’t welcome demands to see more patients.
 Physicians who are mothers are working more—and feeling it.
Physicians who are mothers are working more—and feeling it.
The same JAMA study found physician mothers were the only group to increase weekly work hours, up 3.0% over the past 20 years. Half (49%) of female physicians with parental responsibilities felt very conflicted by work demands, compared with just 28% of physician fathers, according to a January 2023 report by Medscape.
 Relief is a long way off.
Relief is a long way off.
Doctors see a clear solution, a December 2022 survey by InCrowd revealed: In 2022, two-thirds of physicians said hiring more support staff would help, and 55% wanted to reduce the number of patients they saw. But hiring costs, labor shortages, and financial pressures mean employers aren’t planning significant changes in the near term.
How do doctors want their work-life balance issues addressed?
Job satisfaction is a critical barometer for employers of physicians. Despite all the surveys about burnout, 78% of physicians said they would choose to work in medicine again, per a 2022 report by Physicians Thrive. But they still crave better work-life balance.
 Many doctors could use more vacation time.
Many doctors could use more vacation time.
Average time off for most US employees is 10 to 14 days per year, according to the job search platform Indeed. Among doctors, 64% take three or more weeks of vacation each year, but over a quarter (28%) take just one to two weeks, per Medscape’s lifestyle report.
 Doctors say they will take less pay for more autonomy or better work-life balance.
Doctors say they will take less pay for more autonomy or better work-life balance.
Some 71% of doctors told Doximity and Curative that they either already had done so (35%) or would consider it (36%). And according to Medscape, more than half (53%) of doctors said they’d take less money for lighter schedules.
 Some are willing to take more pay for more hours.
Some are willing to take more pay for more hours.
Financial pressures from inflation and reduced Medicare reimbursements are forcing some doctors to think about taking on a side job (33%), increasing their patient caseloads or work hours (14%), or changing employers for a higher salary (11%), per Doximity and Curative.




 Key Takeaways
Key Takeaways

